We stand at a crossroads in healthcare.
Behind us lies a long-lost, nostalgia-tinged world of unfettered physician autonomy, sacred doctor-patient relationships, and a laser-like focus on the art and humanity of medicine. This was the world of my father, an immigrant and Primary Care physician in rural California. The world of Health 1.0.
While many still pine for these “good old days” of medicine, we shouldn’t forget that those days weren’t really all that good. With unfettered autonomy came high costs and spotty quality. Evidence-based medicine didn’t exist; it was consensus and intuition. Volume-based fee-for-service payments incentivized doing things to people, instead of for people. And although the relationship was sacred, the doctor often played the role of captain of the ship, with the rest of the healthcare team and the patients subordinate.
So in response to these shortcomings we now have Health 2.0. The era of Big Medicine. Large corporate groups buying practices and hospitals, managed care and Obamacare, randomized controlled trials and evidence-based guidelines, EMRs, PQRS, HCAHPS, MACRA, Press Ganey, Lean, Six-Sigma. It is the era of Medicine As Machine…of Medicine As Assembly Line. And we—clinicians and patients—are the cogs in the machinery. Instead of ceding authority to physicians, we cede authority to government, administrators, and faceless algorithms. We more often treat a computer screen than a patient. And the doc isn’t the boss, but neither is the rest of the healthcare team—nor the patient. We are ALL treated as commodities…raw materials in the factory of Health 2.0.
And so the calling that brought us into medicine is itself in crisis. 60% of physicians wouldn’t recommend their career to their children, while our nurses are marching on Washington in protest. Why? Because although many of the principles of quality, efficiency, and systems-thinking espoused by Health 2.0 are crucial to moving us forward into the 21st century, we’ve lost the heart and soul of medicine along the way. That distinctly analog human relationship that shifted medicine from career to calling. And nowhere is this more obvious than in Primary Care, ground zero. Thirty-plus patients a day, regulations and paperwork everywhere, dysfunctional EHRs, and patients turning to Dr. Google in despair…is it any wonder that Health 2.0 is breaking the foundation of our healthcare pyramid? My dad could never practice in this dystopia…so he retired.
And yet here I am presenting a music video where I sing, “I hope my children follow Daddy into medicine.”
Why?
Because Health 3.0 is here. In places like Turntable Health, Iora Health, and many others around the country a new emergent path is manifesting…starting with Primary Care. Taking the best aspects of Health 1.0 (deep sacred relationships, physician autonomy) and the key pieces of Health 2.0 (technology, evidence, teams, systems thinking), Health 3.0 restores the human relationship at the heart of healing while bolstering it with a team that revolves around the patient while supporting each other as fellow caregivers. What emerges is vastly greater than the sum of the parts.
Caregivers and patients have the time and space and support to develop deep relationships. Providers hold patients accountable for their health, while empowered patients hold us accountable to be their guides and to know them—and treat them—as unique human beings. Our EHRs bind us and support us, rather than obstruct us. The promise of Big Data is translated to the unique patient in front of us. Our team provides the lift so everything doesn’t fall on one set of shoulders anymore (health coaches, nurses, social workers, lab techs, EVERYONE together). We are evidence-empowered but not evidence-enslaved. We are paid to keep people healthy, not to click boxes while trying to chase an ever-shrinking piece of the healthcare pie. Our administrators seek to grow the entire pie instead, for the benefit of ALL stakeholders…
And so when the family physicians at Health Is Primary asked me if I would be willing to make a video to help the next generation get passionate about the future of Primary Care, I made this. I wanted folks to know that I could honestly tell my daughters that there is no higher calling than every day being with people when they are most vulnerable; getting to know them and their families; preventing illness and alleviating suffering. It is a gift, to get to do what we do every day.
So this is for all of you students out there who are thinking about choosing the family medicine or primary care path. It’s also for all my primary care colleagues who are working hard to make our system better. And it’s for ALL of us in healthcare…we should be proud and inspired as we together forge our way to Health 3.0.
Based on the brilliant original song 7 Years by Lukas Graham. Written and performed by ZDoggMD. Audio engineering by Devin Moore. Directed by Tom Hinueber. Cinematography by Logan Stewart and Variables of Light. Special thanks to Dr. Venu Julapalli for giving us the framework of Health 3.0.
Cast:
- Allison Andersen APRN
- Melat Demeke
- Dave Hart MD
- Stephanie Lapid BSN, RN
- Ken Wong RN
- The ZPupps (my daughters Nina 8 and Maia almost 5)
- Mrs. DoggMD (see if you can spot her!)
Crew:
- Duane Wik
- Steven Z. Smith
- Lindsey Dimick
Join the Health 3.0 movement and watch our daily live Z-Casts on Facebook!
And get me to come perform this LIVE!
7 Years
Once I was 7 years old
My daddy showed me
The path to be a doctor can be lonely
Once I was 7 years old
It was a long tough road, but we thought we were tougher
Pushing each other out the way, as premeds we would suffer
By senior year I bought a suit for interviews, my mother
Was so confused because her son had turned into a gunner
Once I was 20 years old, my daddy told me
“Don’t be a PCP like me, do derm please”
Once I was 20 years old
I always had that dream, like my daddy before me
Be a healer, take the time to know my patients’ story
That subspecialty glory, just always seemed to bore me
To make health primary, that passion always seemed to draw me
Soon I was 30 years old, trapped in a system that sucked souls
Insurance, EHR, Press Ganey owned me
Soon I feel 80 years old
I only see one goal, Health 2.0’s a failure
But I know with all our voices we can make it greater
I got my team with me, our time is now, not later
We love our patients, hate the system, let’s unbreak it major
Once I was 40 years old, our story unfolds
I was finally shown Health 3.0 before me
Once I was 40 years old
Soon I’ll be 50 years old, our practice full grown
We’ve touched thousands of lives but we’re still learning
Soon I’ll be 50 years old
I still marvel at this life
My wife and children awe me
So now I tell them how I’m touched by all my patients’ stories
I got my colleagues with me, we relive that med school glory
And those we lost along the way
My brothers, I’m still sorry
Soon I’ll be sixty years old, my Daddy’d be proud of his son
Remember why we live this life: to make a better one
I made a man so happy when I saved his little son
I hope my children follow daddy into medicine
Soon I’ll be sixty years old, will I look back on the road
And see a job I did, hell no, I’ll see a calling
Soon I’ll be sixty years old
Soon I’ll be sixty years old, will I look back on the road
And see a job I had, hell no, I’ll see a calling
Soon I’ll be sixty years old
Once I was 7 years old
My daddy showed me
The path to be a doctor can be lonely
Once I was 7 years old
Category
- The ZDoggMD Show (818)
- Featured Videos (189)
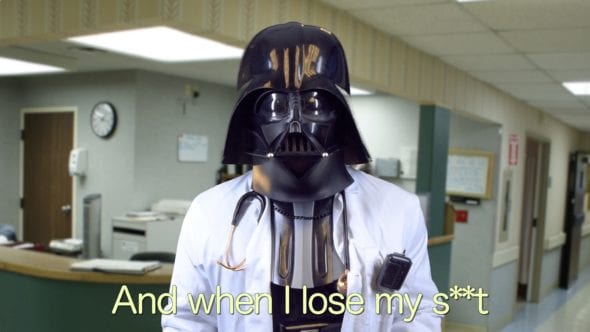
- Doc Vader (142)
- Against Medical Advice (128)
- Medical Humor (95)
- Public Service Announcements (87)
- Music Parodies (74)
- Nurses (59)
- Meditation (46)
- The VPZD Show (38)
- ZVlogg (36)
- ZTalks (28)
- ZBlogg (24)