Another day, another nonsensical battle among health care peeps for who is the biggest douchebag. This is TribeTalk, so hide the kids and cover grandma’s ears BECAUSE IT GETS REAL.
Watch the Facebook LIVE video and make your voice heard!
"Nurse Practitioners are DUMB AND I HATE THEM" #TribeTalk
“Nurse Practitioners are DUMB AND I HATE THEM” #TribeTalk#IncidentReport 106
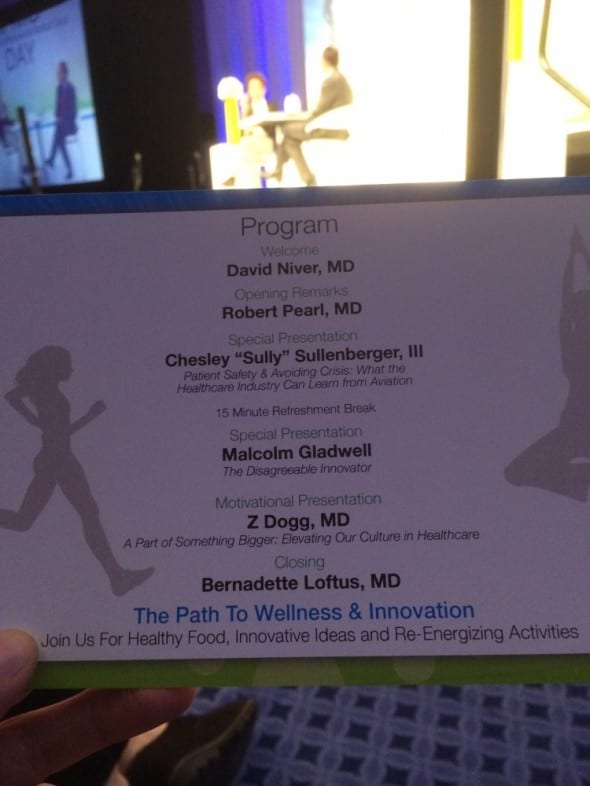
Posted by ZDoggMD on Friday, October 20, 2017
Catch #IncidentReport and Against Medical Advice as a top-rated Science & Medicine podcast on iTunes
Don’t wanna use iTunes? Stream us on Soundcloud or Stitcher.
Support our show and videos on Patreon (your help makes what we do possible)
Shop Amazon using this link (and a portion of the proceeds goes to support the show)
We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites. Check out ZDogg’s recommended books and gear here!
Learn about direct sponsorship opportunities
Sign up for our weekly email video summary
Category
- The ZDoggMD Show (818)
- Featured Videos (189)
- Doc Vader (142)
- Against Medical Advice (128)
- Medical Humor (95)
- Public Service Announcements (87)
- Music Parodies (74)
- Nurses (59)
- Meditation (46)
- The VPZD Show (38)
- ZVlogg (36)
- ZTalks (28)
- ZBlogg (24)